Have an Apple Watch and want to start the CHOP protocol for POTS today? Try the new POTS exercise program in Empirical Health for Apple Watch.
Where did the CHOP protocol come from?
The Children’s Hospital of Philadelphia (CHOP) protocol is an exercise routine that was adapted from Dr. Benjamin Levine’s research on how exercise affects patients with postural orthostatic tachycardia syndrome (POTS). Dr. Levine, a sports cardiologist and the founding director of the Institute for Exercise and Environmental Medicine at Texas Health Presbyterian Hospital Dallas, has focused his career on exploring how circulation adapts in response to various factors, including exercise, aging, and environmental stimuli. Over the course of his career Dr. Levine and his team have conducted research on the impact of exercise on human physiology - this has helped build the foundation for helping us understand the role of exercise in POTS.
You may have heard this protocol referred to by different names: Levine protocol, modified CHOP protocol, Dallas protocol, etc. While these may have slight variations from the initial protocol defined by Levine, they are all rooted on the same principle.

How does the CHOP protocol for POTS work?
Dr. Levine’s research suggests that people with POTS are no different than people without POTS – everyone’s exercise performance improves with exercise conditioning. More specifically, research in this area has shown that a dedicated exercise protocol could lead to significant improvement in symptoms for a lot of POTS patients.
In one of Levine’s studies, the researchers coached people with POTS through a 3-month exercise program. The program was designed to accommodate for orthostatic intolerance. As such, people began with 3 weekly sessions of sitting exercises (rowing, swimming, or recumbent bike) for 20-30 minutes targeting specific heart rate zones. Over time the participants increased their activity with longer sessions and eventually more weekly sessions. By the third month of training upright exercise was also incorporated. In addition, people participated in weekly strength training consisting of light weightlifting for 15-20 minutes. The research team found that 53% of participants did not meet the criteria for POTS after the 3-month exercise program and they showed gains in their peak oxygen uptake, cardiac mass, and blood volume. The ability of the heart to pump blood at each beat improved with the training program.
Interestingly, Dr. Levine’s research team has also completed smaller studies that suggest exercise may be superior to beta blockers in regard to improving standing heart rate and quality of life.

How do I incorporate the CHOP protocol into my own treatment program?
You don’t need to have formal coaching to benefit from similar positive effects outside of a research environment.
Generally there are a few guidelines to follow:
-
Start slow and pace yourself : recumbent exercise at a lower pace will be a more accessible entry point for a lot of POTS patients. Over time, you will be able to tolerate more frequency and intensity of activity.
-
Be consistent : your body requires activity to remain strong; pausing your exercise program will lead to some loss of the gains you have made even after just a few days. Spreading your exercise sessions throughout the week can help avoid this.
-
Mix aerobic exercise with strength training : both of these types of exercise work in synergy to improve your cardiac conditioning and your overall muscle strength.
-
Be patient and kind to yourself : it will take time to see a noticeable difference with any exercise program. This can be frustrating when you’re not feeling well. If you need to take a break, that’s ok! The training program can always be restarted when you are ready - just make sure to restart slowly.
How to start the CHOP protocol for POTS
If you have an Apple Watch, we’ve created a POTS exercise program that you can do at home. You can choose your preferred exercise, then preload workouts onto your Apple Watch. It supports both heart rate zones and self-rated exertion (for those on beta blockers):
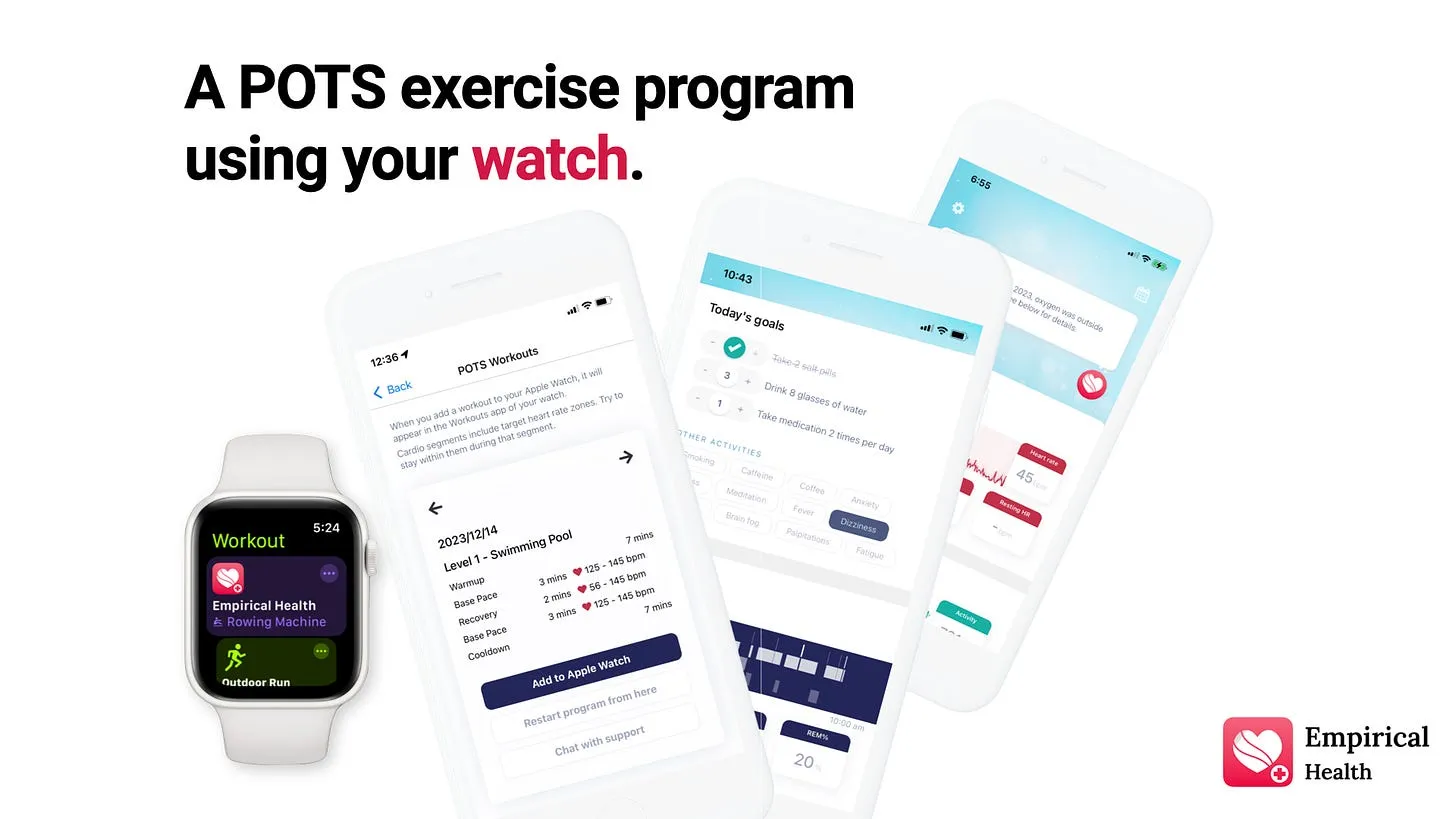
To get started, download Empirical Health on the App Store. Let us know what you think!
Get your free 30-day heart health guide
Evidence-based steps to optimize your heart health.
